Quisiera sugerir una reflexión a propósito del accidente isquémico transitorio (AIT) (TIA) (transient ischemic attack). Es un reflexión extensible a todos los ámbitos de la Medicina, especialmente en los países donde tenemos la fortuna de tener un sistema sanitario público. Es una reflexión sobre el gasto sanitario. Sobre prioridades. Sobre demagogias y votos. Sobre la dura realidad.
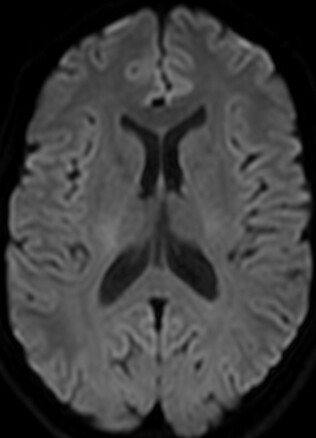
Hace ya demasiados años, cuando estaba en la Facultad de Medicina, reputados neurólogos me enseñaron que un accidente isquémico transitorio es un episodio de disfunción neurológica de origen isquémico que dura menos de 24 horas. Imagino que la mayoría de los lectores tendrán esta misma idea. Bien. Las cosas cambian. Aumenta el conocimiento. Se generaliza la utilización de secuencias de difusión en resonancia. Un buen día la Asociación Americana del Corazón (American Heart Association) propone un pequeño cambio en la definición de AIT. Añade una cláusula. Para ser un AIT debe demostrase la ausencia de infarto.
Stroke. 2009 Jun;40(6):2276-93. Epub 2009 May 7.
Abstract
This scientific statement is intended for use by physicians and allied health personnel caring for patients with transient ischemic attacks. Formal evidence review included a structured literature search of Medline from 1990 to June 2007 and data synthesis employing evidence tables, meta-analyses, and pooled analysis of individual patient-level data. The review supported endorsement of the following, tissue-based definition of transient ischemic attack (TIA): a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction. Patients with TIAs are at high risk of early stroke, and their risk may be stratified by clinical scale, vessel imaging, and diffusion magnetic resonance imaging. Diagnostic recommendations include: TIA patients should undergo neuroimaging evaluation within 24 hours of symptom onset, preferably with magnetic resonance imaging, including diffusion sequences; noninvasive imaging of the cervical vessels should be performed and noninvasive imaging of intracranial vessels is reasonable; electrocardiography should occur as soon as possible after TIA and prolonged cardiac monitoring and echocardiography are reasonable in patients in whom the vascular etiology is not yet identified; routine blood tests are reasonable; and it is reasonable to hospitalize patients with TIA if they present within 72 hours and have an ABCD(2) score >or=3, indicating high risk of early recurrence, or the evaluation cannot be rapidly completed on an outpatient basis.
No está mal. Va con los tiempos. Pero me gustaría llamar la atención sobre el hecho de que este sencillo cambio puede acarrear la necesidad de realizar un montón de resonancias magnéticas más de las que venimos haciendo, que no siendo pocas, son muchas menos de las que deberíamos hacer. Y me surgen varias preguntas: ¿nos encontramos en posesión de la infraestructura necesaria para poder cumplir este cometido?, si hacemos las cosas bien, ¿podría el gasto ascender hasta límites insostenibles? ¿qué medidas habría que tomar para evitarlo? ¿descatalogar prestaciones? ¿cobrar por algunas prestaciones? ¿copago? ¿podemos asumir y concienciar a la población de que en nuestro sistema sanitario se deben usar diferentes algoritmos diagnósticos o terapéuticos por motivaciones económicas?
Stroke. 2010 Aug 26. [Epub ahead of print]
How Much Would Performing Diffusion-Weighted Imaging for All Transient Ischemic Attacks Increase MRI Utilization?
Adeoye O, Heitsch L, Moomaw CJ, Alwell K, Khoury J, Woo D, Flaherty ML, Ferioli S, Khatri P, Broderick JP, Kissela BM, Kleindorfer D.
From University of Cincinnati Neuroscience Institute, Cincinnati, Ohio; Department of Emergency Medicine, University of Cincinnati, Cincinnati, Ohio; Department of Neurosurgery, University of Cincinnati, Cincinnati, OH; Department of Neurology, University of Cincinnati, Cincinnati, Ohio; Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio.
Abstract
Objectives-The American Heart Association recently redefined TIA to exclude patients with infarction on neuroimaging. Given its advantages, MRI/diffusion-weighted imaging (DWI) was recommended as the preferred imaging modality. We determined how frequently MRI/DWI was performed for TIA and ascertained the proportion of clinically defined TIA patients who had ischemic lesions on DWI in our community in 2005.
METHODS: All clinically defined TIA cases among residents of a 5-county region around Cincinnati who presented to emergency departments were identified during 2005. Demographics and medical history, whether MRI/DWI was performed, and DWI findings were recorded. Generalized estimating equations were used to compare groups to account for the design of the study and multiple events per patient.
RESULTS: Of 834 TIA events in 799 patients, 323 events (40%) had MRI/DWI performed. Patients who had MRI/DWI were younger (mean, 66 vs 70 years; P=0.03), had less severe prestroke disability (baseline modified Rankin Scale score, 0; 44% vs 34%; P=0.02), were less likely to have previous stroke or TIA (42% vs 56%; P=0.002), and were less likely to have atrial fibrillation (10% vs 16%; P=0.01). Of the 323 events with DWI, 51 (15%) had evidence of acute infarction. Patients with positive DWI were older (75 vs 64 years; P=0.0001) and more likely to have atrial fibrillation (21% vs 7%; P=0.002).
CONCLUSIONS: Performing MRI/DWI on all clinically defined TIA patients in our community would reveal more cases of actual infarction but would more than double current use. Future studies should assess whether MRI/DWI is warranted for all TIA patients.

No hay comentarios:
Publicar un comentario