Diffusion-weighted MRI in acute stroke within the first 6 hours. 1.5 or 3.0 Tesla?
From the AP-HP, Urgences Cérébro-Vasculaires (C.R., G.M., C.P., Y.S.), and AP-HP, Service de Neuroradiologie (A.D., D.L., S.L., D.D.), Université Pierre et Marie Curie, Paris VI, Hôpital Pitié-Salpêtrière, Paris, France.
Abstract
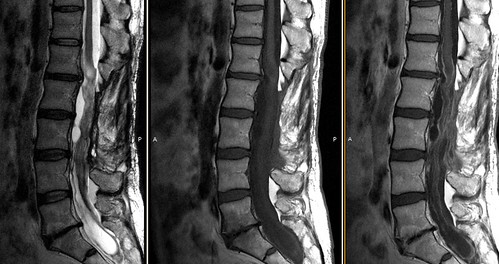
OBJECTIVES: To compare the sensitivity and specificity of 1.5-T and 3.0-T diffusion-weighted MRI (DWI) to detect hyperacute ischemic stroke lesions. METHODS: We blindly reviewed the DWI of 135 acute stroke patients and 34 controls performed at 1.5 T (n = 108) or 3.0 T (n = 61). The stroke patients all had subsequently proved carotid territory ischemic stroke and were imaged within the first 6 hours after stroke onset. Four readers (2 neuroradiologists and 2 stroke neurologists) blinded to clinical data and magnetic field strength recorded the presence of ischemic lesions on DWI and apparent diffusion coefficient (ADC) maps if necessary. Sensitivity, specificity, and false-negative rates were computed. Signal-to-noise ratio (SNR), contrast-to-noise ratio (CNR), and DWI contrasts were calculated at both field strengths. RESULTS: The accuracy of DWI in stroke diagnosis was superior at 1.5 T (98.8%) than at 3.0 T (90.9%, p = 0.03). The sensitivity decreased from 99.1% at 1.5 T to 92.5% at 3.0 T (p = 0.06) and the specificity from 97.8% to 84.1% (p = 0.002). ADC map readings did not improve accuracy, sensitivity, or specificity. The false-negative rate was 0.6% at 1.5 T and 6.1% at 3.0 T. Type of readers, stroke severity, and type of the coil did not affect diagnosis value. SNR and CNR were significantly higher at 3 T (p < 0.0001) but DWI contrast was lower (p = 0.04). CONCLUSIONS: Blind reading by 4 experts of a large series of images shows that 1.5-T diffusion-weighted MRI (DWI) is better than 3.0-T DWI for the imaging of hyperacute stroke during the therapeutic window of thrombolysis.
Vaya, vaya. Seguimos con la línea de artículos ligeramente sorprendentes, aunque no tanto. O sea que la resonancia de 3.0 T no es tan buena como el viejo cacharro de 1.5 T para el infarto hiperagudo. Espero que no empiecen a salir publicaciones de este tipo para otros tipos de exploraciones o situaciones clínicas. Aunque soy escéptico por naturaleza. Estoy seguro, no obstante, de que el mayor número de artículos defenderá los avances y progresos que con toda seguridad se van a obtener de la nueva máquina, pero se agradece una bocanada de aire fresco de gente con capacidad crítica que compense el efecto "¡ta-chan!" de la novedad tecnológica. Aprovecho para recordaros que si queréis opinar o discrepar o advertir que vuestros datos no coinciden con los de los autores del artículo, podéis hacerlo enviando un comentario.